OVERVIEW
STUDY DATES: 2020 – 2025
Research Title: Modeling Reductions in Harmful Alcohol Use on HIV Transmission and Mortality in the Era of Universal Test and Treat in Uganda
This project will improve understanding of the relationship between harmful alcohol use and the HIV epidemic through the following study aims.

STUDY AIMS
Aim 1: Estimate the prevalence of harmful alcohol use and relationships with receipt of ART and viral load suppression in the era of universal test and treat (UTT) in Uganda.
Aim 2: Quantify the contribution of harmful alcohol use to HIV transmissions and mortality in Uganda during the UTT era, using infectious disease modeling.
Aim 3: Determine the cost-effectiveness of alcohol reduction interventions to prevent HIV transmission, in Uganda.

WHY?
The World Health Organization (WHO) recommends that all people living with HIV (PLWH) initiate ART and countries in sub-Saharan Africa (SSA) have rolled out a universal test and treat (UTT) strategy. Some recent trials have shown that expanded treatment does not always result in reduced HIV incidence at the population level. Questions remain on the role of underlying factors that may reduce the benefits of UTT and drive the HIV epidemic. According to a recent UNAIDS report, alcohol use is an overlooked factor in the HIV epidemic that requires greater attention. Alcohol use increases HIV risk through sexual behaviors and reducing uptake and adherence to ART. Thus, alcohol use may contribute to population-level failure to achieve HIV elimination targets. This research will estimate the long-term, population impact of harmful alcohol use on HIV transmission and mortality in the UTT era in Uganda. Uganda has one of the highest levels of alcohol use per capita in SSA and has a generalized HIV epidemic, with a prevalence of 5.7%. The UTT strategy took effect in Uganda in 2017. However, in 2019, 22% of PWH in Uganda were not on ART and 36% were not virally suppressed. Uganda has an opportunity to address both burdens by reducing harmful alcohol use. This research will assess the value for money of investing in alcohol use interventions to reduce HIV transmission in the era of UTT in Uganda.
Principal Investigators (PIs)
Adriane Wynn, PhD1
Collaborating local mentor: Noah Kiwanuka, PhD2
PI Affiliations
1University of California
San Diego, California, USA
2Makerere University School of Public Health
Kampala, Uganda
LOCATION
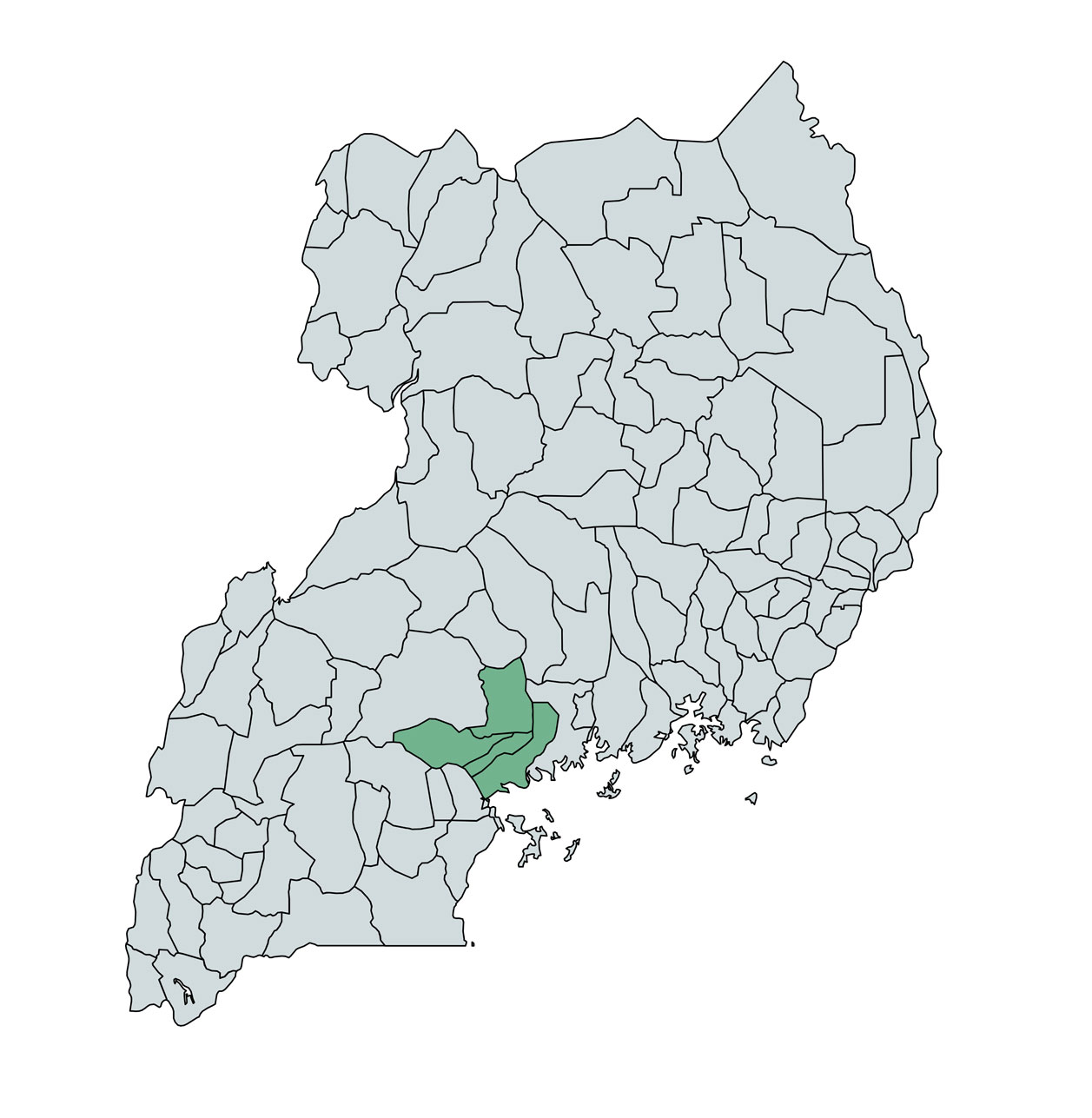
Existing data from a study in Mpigi, Butambala, Gomba, and Mityana Districts, Uganda
FUNDER: National Institute on Alcohol Abuse and Alcoholism, K01AA027733
Contact us with any inquiries or questions
OUTCOMES
Wynn, A., Sileo, K. M., Schmarje Crockett, K., Naigino, R., Ediau, M., Menzies, N. A., Kalichman, S. C., Wanyenze, R. K., Martin, N. K., & Kiene, S. M. (2024). Associations between alcohol, antiretroviral therapy use, and viral load suppression among people living with HIV in rural Central Uganda. AIDS and Behavior, 28, 2205-2215. https://doi.org/10.1007/s10461-024-04299-x
Wynn, A., Sileo, K. M., Schmarje Crockett, K., Naigino, R., Ediau, M., Wanyenze, R. K., Kiwanuka, N., Martin, N. K., & Kiene, S. M. (2024). Prevalence of alcohol use by gender and HIV status in rural Uganda. PLOS ONE, 19(7), e0303885. https://doi.org/10.1371/journal.pone.0303885
Building Research Initiatives Advancing Global Health Equity (BRIDGE) at San Diego State University

