OVERVIEW
STUDY DATES: 2024 – 2025
Research Title: Boosting maternal vaccination in Uganda: Insights from antenatal care providers in a high burden, low resource setting
In line with the imperative to attain global vaccine equity, this research will gather healthcare providers’ views on why people in Uganda low confidence in vaccines and what obstacles may have they face in getting vaccinated. The goal is to improve vaccination programs, especially for mothers and infants in a region characterized by a high HIV prevalence and limited resources. Using qualitative methods (40 in-depth interviews), we will conduct a pre-implementation assessment to understand provider perspectives on barriers to maternal immunization in the current landscape as well as the acceptability, feasibility, and appropriateness of expanding the maternal immunization program and identifying optimal strategies for delivery of maternal vaccination in this context. Interviews will be conducted with providers serving women living with and without HIV at facilities across two of Uganda’s districts. The proposed work will serve as the first phase of a body of formative research aimed at identifying modifiable factors that can be targeted to address gaps in immunization coverage and improve maternal commitment to vaccination, not only during pregnancy but for their
children as well.
STUDY AIM
Identify opportunities for and barriers to successful implementation of maternal and neonatal vaccination programming including the use of monoclonals.
WHY?
Comprehensive immunization programs can significantly reduce the burden of disease attributable to vaccine preventable diseases across the lifespan. The continent of Africa, which is home to 1.3 billion people, has the lowest vaccination coverage rates globally. Although there have been major strides in vaccine coverage in sub-Saharan Africa, as evidenced by the reduction in measles-related deaths over the past twenty years barriers to achieving optimal coverage persist; namely, challenges related to care seeking patterns and vaccine hesitancy. To overcome barriers to vaccine uptake, it is critical to understand contextual and cultural factors that contribute to poor uptake and hesitancy from the perspectives of multilevel stakeholders. Healthcare providers can offer valuable insights into individual and structural factors driving vaccine hesitancy and low vaccination rates. They can also identify anticipated barriers around the introduction of novel vaccines and monoclonals which can inform delivery strategies and programmatic messaging.
Uganda serves as an ideal case study for other LMICs because it creates an opportunity to consider immunization programming in real world context under conditions that are characteristic of many LMICs, including: limited health infrastructure, suboptimal antenatal care engagement, low levels of health literacy, and a high prevalence of co-morbidities (such as HIV) which may have implications for both attitudes towards vaccination/monoclonals as well as maternal vaccine efficacy. We anticipate that the results from this study will not only benefit immunization efforts in Uganda but provide valuable preliminary data for identification of programmatic roll out approaches that can maximize the reach of maternal and pediatric vaccination/monoclonal delivery campaigns in similar contexts.
Principal Investigators (PIs)
Susan M. Kiene, PhD, MPH1
Amanda P. Miller, PhD, MS1
Gertrude Nakigozi, PhD, MPH2
PI Affiliations
1San Diego State University
San Diego, California, USA
2Africa Medical and Behavioral Sciences Organization, Wakiso, Uganda
PARTNERS
- Africa Medical and Behavioral Sciences Organization, Wakiso

LOCATION
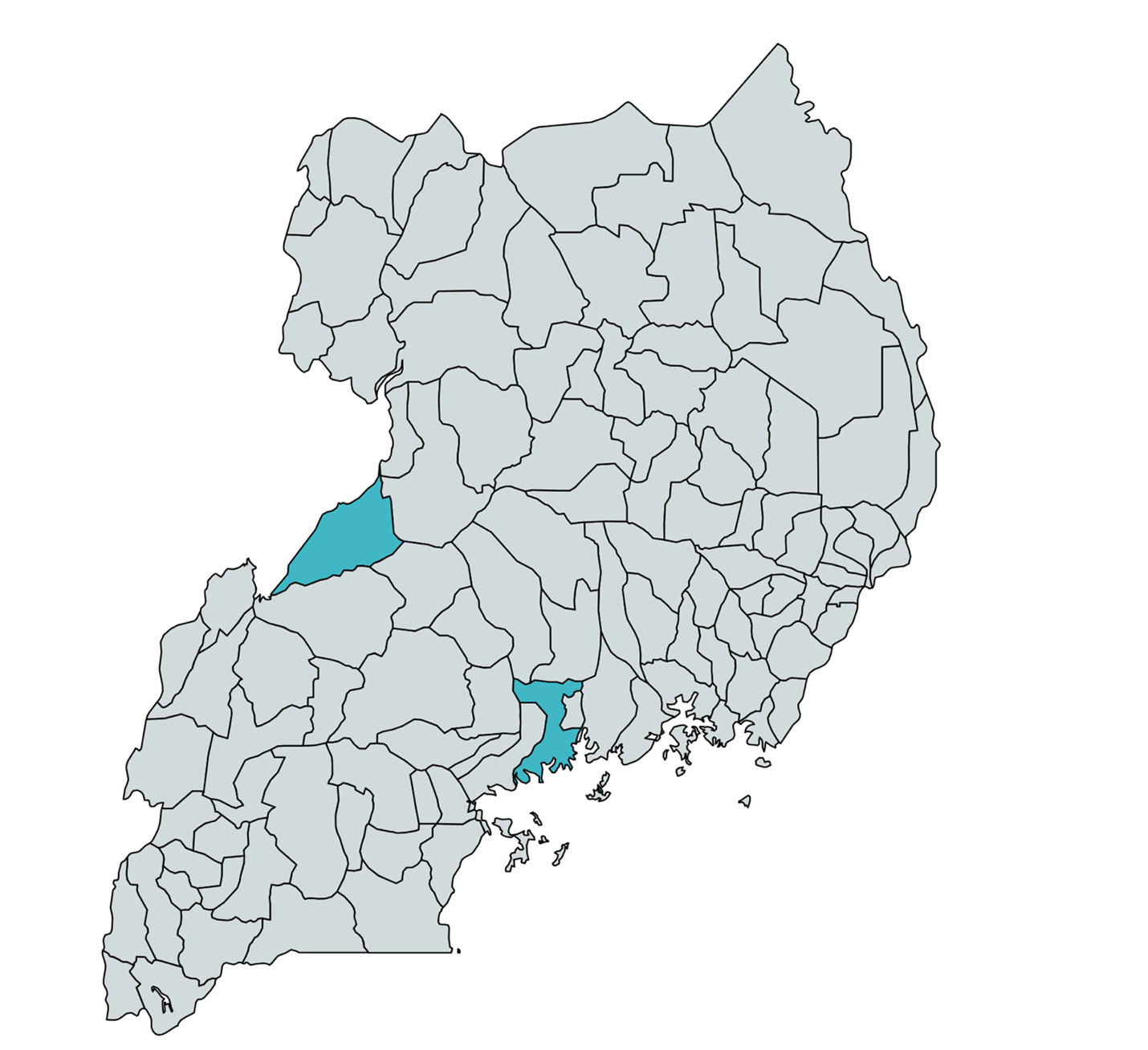
Wakiso and Hoima Districts, Uganda
FUNDER: Merck Investigator Studies Program
Contact us with any inquiries or questions
OUTCOMES
Stay tuned…
Building Research Initiatives Advancing Global Health Equity (BRIDGE) at San Diego State University

