OVERVIEW
STUDY DATES: 2024 – 2029
Research Title: Reducing hazardous alcohol use and optimizing treatment as prevention among men living with HIV in risk environments
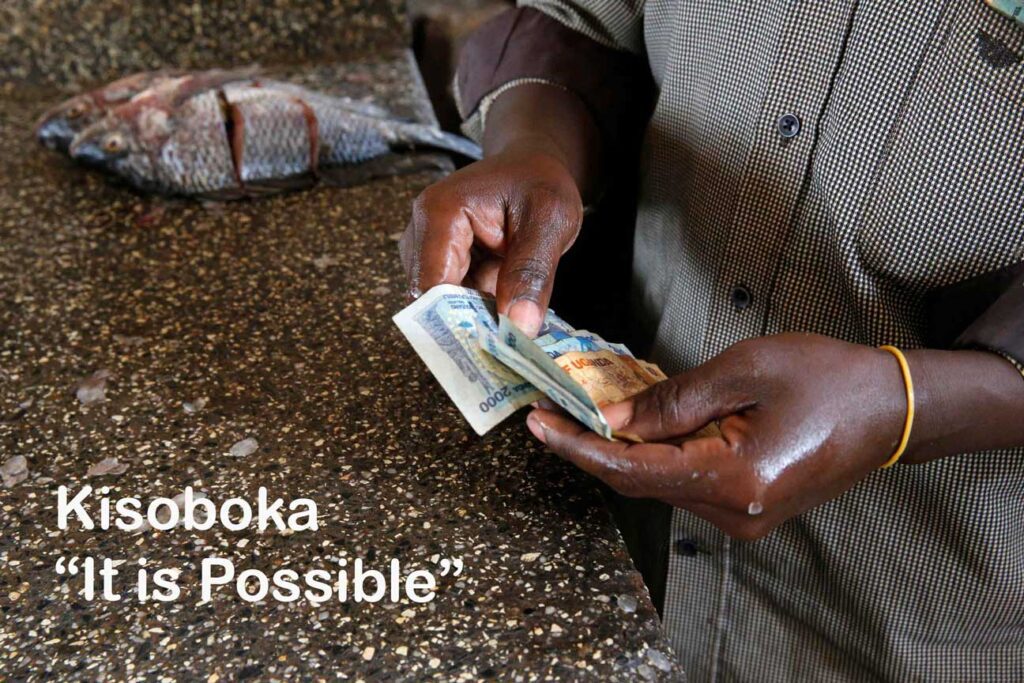
We developed Kisoboka (“It is Possible”), a behavioral intervention adapted from two evidence-based interventions and included a structural element to “reduce cash in the pocket” easily accessible for alcohol purchase and to promote savings. Kisoboka utilizes a behavioral economics approach and motivational interviewing to reduce hazardous drinking and improve antiretroviral (ART) adherence to achieve undetectable HIV viral load (VL).
STUDY AIMS
Aim 1. Determine the efficacy of the Kisoboka intervention and its components on alcohol and HIV outcomes among hazardously drinking men living with HIV in Uganda in a 2×2 factorial randomized control trial.
Aim 2. Assess the impact of the Kisoboka intervention and its components on measures of psychological, physical, and socioeconomic well-being that capture frequent comorbidities of persons living with HIV and are associated with achieving successful treatment as prevention.
Aim 3. Understand barriers and facilitators in the inner and outer context for implementing the components of Kisoboka within the routine clinical setting to inform future widespread implementation.

WHY?
We developed the Kisoboka (“It is possible”) Intervention to address limitations of existing evidence-based interventions to optimize treatment as prevention among men living with HIV (LWH) who are hazardous alcohol users in “risk environments” such as fishing communities through reductions in hazardous alcohol use, improved ART adherence and achieving undetectable viral loads.
Social and structural determinants unique to fishing communities interact to create a risk environment where hazardous drinking impedes ART adherence among men LWH, including prevalent social norms of drinking, drinking as a way of experiencing “reward” and connecting with others (e.g. in the context of transactional sex), stressful work conditions, a “live for today” outlook, and a cash-based economy with no traditional savings infrastructure leading to ease of daily expenditure on drinking and sex work. These social and environmental conditions result in high levels of alcohol misuse and HIV risk, poor HIV outcomes, and exacerbation of HIV-associated wellness comorbidities such as poor mental and subjective physical health and food insecurity. Optimal ART adherence and treatment as prevention among fisherfolk LWH and other key populations remains a challenge, underscoring the need for interventions specifically tailored for this and similar risk environments.
Principal Investigators (PIs)
Susan M. Kiene, PhD, MPH1
Joseph Matovu, MHS, PhD2
PI Affiliations
1San Diego State University School of Public Health
San Diego, California, USA
2Makerere University School of Public Health
Kampala, Uganda
PARTNERS
- Mildmay Uganda
- University of California, San Francisco
- Makerere University Walter Reed Project
- Boston College

LOCATION
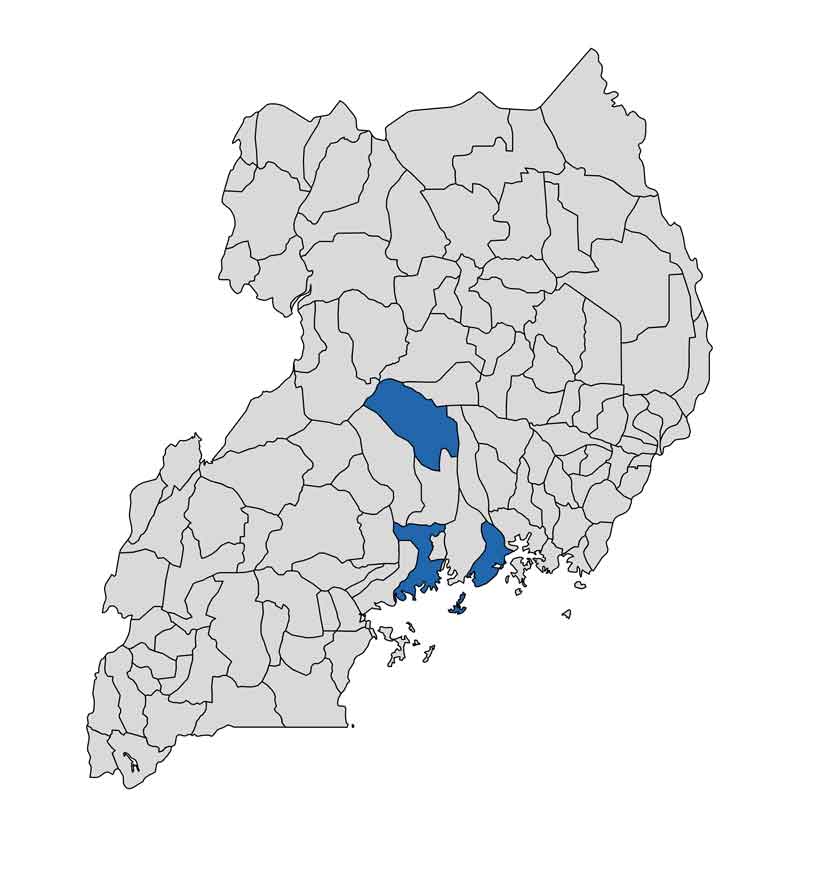
Wakiso, Nakasongola, and Buikwe District fishing communities along Lake Victoria and Lake Kyoga in Uganda
FUNDER: NIH, National Institute on Alcohol Abuse and Alcoholism
Contact us with any inquiries or questions
OUTCOMES
Stay tuned …
Building Research Initiatives Advancing Global Health Equity (BRIDGE) at San Diego State University

